Leveraging PEPFAR Data Systems to Strengthen National Health Information Systems
By Pascal Mwele

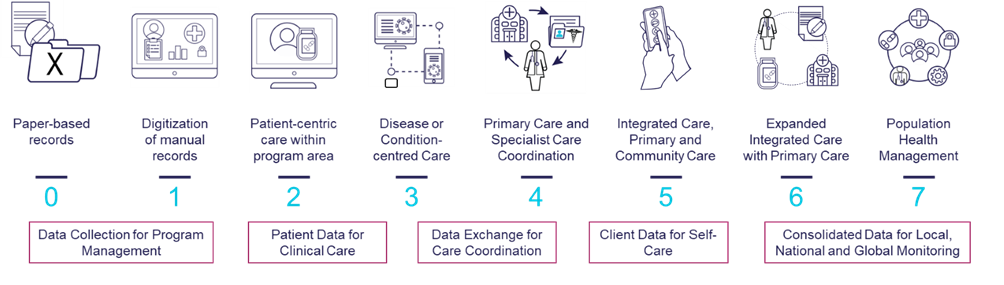
In 2014, the Healthcare Information and Management Systems Society (HIMSS) developed the Continuity of Care Maturity Model (CCMM) to assist healthcare leaders worldwide in assessing, implementing, and scaling seamless patient care coordination across multiple care sites and providers. The CCMM provides a framework of seven idealized stages for value-based and client-centered care to support the evolution of different digital health systems.
While not created specifically for HIV programs, the CCMM has become especially relevant for those working on U.S. President’s Emergency Plan for AIDS Relief (PEPFAR)-supported digital systems. Originally designed to collect raw data, PEPFAR systems are increasingly being redesigned to be more people-focused, with an emphasis on client interfaces and point-of-care integration, including primary healthcare needs. The CCMM helps us to think through the ultimate goals of such redesigns, as well as identify areas where deliberate attention is required.
Despite some countries’ rapid build-up of their digital health systems in line with the later stages of the CCMM, others still lack the necessary infrastructure and governance frameworks.
In these cases, existing PEPFAR systems can be a vital steppingstone for broader reconfigurations in the national health information system (HIS). Transformative change that maintains local ownership is possible if PEPFAR investments are reconfigured to meet evolving healthcare needs and realigned with unified country architecture.
Our Experience
Within this context, the Data for Implementation (Data.FI) project and our partners seek to optimize HIS within the primary healthcare environment by enhancing existing digital health investments. This happens at multiple levels—including supporting electronic medical record (EMR) systems, as well as community-based, laboratory, commodity tracking, and pharmacy systems.

In the process of doing this work across multiple countries, we have gained critical insights.
For instance, while the move from paper-based records to digital systems, such as EMRs, has had a positive impact, a holistic, client-centered approach is often lacking. It is only possible to achieve this when the current siloed, HIV-specific systems and processes are reengineered and expanded to support clinical care workflows in various operational contexts.
In addition, unique personal identification and interoperability play an important role in ensuring effective healthcare delivery across expanded clinical care service points. Data.FI has always applied pragmatic approaches customized to the country context, as there is no one-size-fits-all solution.
Also, we have found that low-resource implementation contexts require more than digital evolution; instead of introducing technology for its own sake, revolutionary processes and product innovations are required. More specifically, implementers must refine existing PEPFAR-supported digital health investments to support primary healthcare ecosystems.
Our Learnings: Key Principles for HIS Expansion
Beyond these broad insights, Data.FI has produced six key principles for how to leverage PEPFAR systems to expand and enhance HIS in a way that accommodates local and national government priorities:
Strategic alignment: As existing systems are expanded to accommodate additional use cases; the effort should align with local and national priorities. When HIS investments are aligned with government goals, they deliver more value, promote ownership, and attract government investment. For instance, if a country has an eHealth strategy, donors and implementing partners must consider how the HIS investments align with the government enterprise architecture and allocate complementary financial and non-financial resources through strategic alignment. The result is a higher return on investment and a better use of time and effort.
Design for person-centered system evolution: Once HIS initiatives have strategic alignment, ensure that HIS are re-engineered for a shift from a siloed, monolithic data-centric design to a service-oriented, people-centric design. HIS design needs to adapt with user needs, health sector goals, and technology landscape changes. HIS relevance, user-friendliness, and optimization can be achieved through evolutionary design. Additionally, this approach reduces the likelihood of future large-scale redesigns, which can be disruptive and costly.
Standards-based software integration and interoperability: In today's digital ecosystem, software rarely operates in isolation. It is increasingly important to integrate diverse HIS components, such as EMRs, with community outreach programs, laboratories, and pharmacies in a seamless manner as the health sector transitions to primary healthcare models. Communication between different software systems is key to delivering seamless user experiences and simplifying clinical care or public health response operations. Integrating and interoperating software based on standards also ensures that updated software can easily interface with other evolving systems, databases, and third-party services, reducing data silos and increasing efficiency.
Management and protection of data: As systems become more interconnected and data elements become more granular, prioritizing responsible data management and protection isn't just a procedural necessity; it's a commitment to safeguarding the privacy and trust of countless individuals. The ability to consolidate, analyze, and visualize data is as important as safeguarding it effectively and efficiently. Having this proficiency produces accurate, actionable insights that shape service delivery and health outcomes. Data management also facilitates access to reliable, usable data for decision making by ensuring that the right data is accessible to the right users. It is important to manage and protect data to foster trust among users, promote HIS utility and avoid costly data protection regulatory violations.
Implementing innovative solutions: To align with different local contexts' strategic and regulatory requirements, thus ensuring that system designs are progressive, interoperable, and adaptable to unique user needs, innovative solutions are essential. Extended HIS use cases can be differentiated from previous siloed implementations by embracing adaptable technologies, methodologies, and design patterns.
Continuous evaluation and implementation: The dynamic nature of user needs, coupled with technological advancements, necessitate continuous feedback loops in software development. Iterative improvements to HIS software can be made by continuously evaluating software performance, user feedback, and emerging technology trends. As a result, the HIS is always optimized, bugs are addressed promptly, and the product is aligned with users' evolving needs.
The progression to a fully mature HIS is never linear or simple. But by leveraging PEPFAR investments and following deliberate, holistic principles, progress toward an integrated HIS can be achieved more quickly.


